Navigating life with
EoE

Talking about your EoE
Eosinophilic esophagitis (EoE) can be hard to explain, especially when it shows up in conversations you didn’t expect. This guide walks you through real scenarios and gives you simple, practical ways to talk about what you’re going through. The goal isn’t to say everything perfectly. It’s to feel more understood and confident speaking up when it matters.
Talking to your server at a restaurant
Eating out with EoE can be difficult, but with the right tools and preparation, you can enjoy meals away from home safely. Let your server know about your needs early, using clear and direct language.
Before you order
Server: “Are there any allergies or dietary restrictions we should know about?”
You: “I have a medical condition that requires me to avoid certain foods, and I need to be very careful about cross-contact with allergens such as (note your personal food triggers).”
Note: If it’s more comfortable for you, it’s okay to tell your server that you have a food allergy—even if it’s not entirely accurate. The word “allergy” signals to servers that what you are saying is serious and needs attention.
When you order
Server: “What can I get for you?”
You: “I’m thinking of ordering X (choose a dish that looks safe for you to eat). Can you please confirm what the preparation process is and if there are any unlisted ingredients, like X (note your personal food triggers)?”
When your food arrives
Server: “Enjoy your meal!”
You: “Thank you! I wanted to double check that this dish doesn’t have X (note your personal food triggers) in it?”
Having a meal with an acquaintance
If you’re in a dining situation with someone you don’t know well, you may not need to explicitly mention your EoE. Remember, you can keep your explanation simple and only share what you feel comfortable with.
Acquaintance: “Do you want to split some appetizers?”
You:
- “I have some food allergies, so I ate before coming. You guys order what you want!”
- “I have some food allergies. The appetizers I can eat on the menu are [insert foods], if any of those sound good to you!”
Talking about EoE at work
Many people have never heard of EoE, which can make it feel awkward to explain. Practicing a simple way to describe your condition can help your manager and coworkers understand and reduce the pressure you feel.
You:“I have eosinophilic esophagitis, or EoE. It’s a chronic condition that causes inflammation in my esophagus, triggered by certain foods or allergens. I [select which are relevant for you: follow a strict diet; experience symptoms like trouble eating certain foods, chronic fatigue and nausea; have to take medicine regularly]. This means I may need to bring my own food, store my medication in the office, take breaks, or adjust my schedule for appointments. It’s manageable, but I appreciate your understanding when I need flexibility.”
Manager: “Thank you for sharing this with me. I want to make sure we support you in managing your health while at work. Let’s talk about what specific accommodations or flexibility you might need.”
Sharing with your partner
Open communication with your partner is key to building understanding and support. It’s important to share details about your experience with EoE so your partner can help you feel comfortable.
You: “I want to share something important with you. I have a medical condition called eosinophilic esophagitis, or EoE. It means my esophagus can get inflamed, often because of certain foods or allergies, and it sometimes makes swallowing difficult and eating out a bit tricky for me.”
Partner: “Thank you for telling me. How can I support you?”
You (topic: food): “I have to be careful with what I eat, and sometimes I might need to bring my own food or ask for accommodations at a restaurant. It can feel frustrating at times, so I appreciate your patience if I seem anxious or cautious around food and social events.”
You (topic: medication): “I take medication to help manage my EoE, but I can still have symptoms like trouble swallowing, fatigue, or nausea. These can affect my energy levels or how I feel day to day. Sometimes I might need to rest more, change plans, or take extra care when we’re out together.”
Talking to your roommate
Sharing information about your EoE with your roommate can help ensure your safety and comfort. Letting them know about your dietary needs, medication routines, location of treatments such as EpiPens, and what to do in case of an emergency can prevent misunderstandings and make it easier to manage your health while living together. Open communication helps your roommate support you, especially if you have specific food restrictions in shared spaces.
You (topic: food): “I want to talk to you about something important regarding my health. I have a chronic condition called eosinophilic esophagitis, or EoE, which affects my esophagus and makes me sensitive to certain foods. I have to follow some specific dietary restrictions to avoid symptoms, which can sometimes be triggered by cross-contact. Can we talk about shared spaces, like the kitchen, and what we both need in terms of food prep and storage?”
You (topic: medication and emergencies): “I take meds to help keep my EoE under control, but I still get flare-ups sometimes. Some of my meds have to be kept in the fridge or in a certain spot, so I try to stay on top of that. If I start having symptoms or there’s an emergency, I’ll let you know what to watch for and what to do—just so we’re both on the same page and prepared.”
Roommate: “Yes, thank you for letting me know!”
At an appointment with your primary care provider
Being open and honest about your EoE with your primary care provider is essential for getting the best possible care. Sharing more about EoE and how it impacts your daily life will help them understand how EoE affects your overall health.
Primary care provider: “Do you have any health updates you would like to share with me?”
You: “Yes, I’ve been diagnosed with eosinophilic esophagitis, or EoE, a chronic condition that affects my esophagus and my quality of life overall. I know it’s not very common, so I wanted to share a bit about my experience managing my symptoms.”
Going out to eat with
EoE
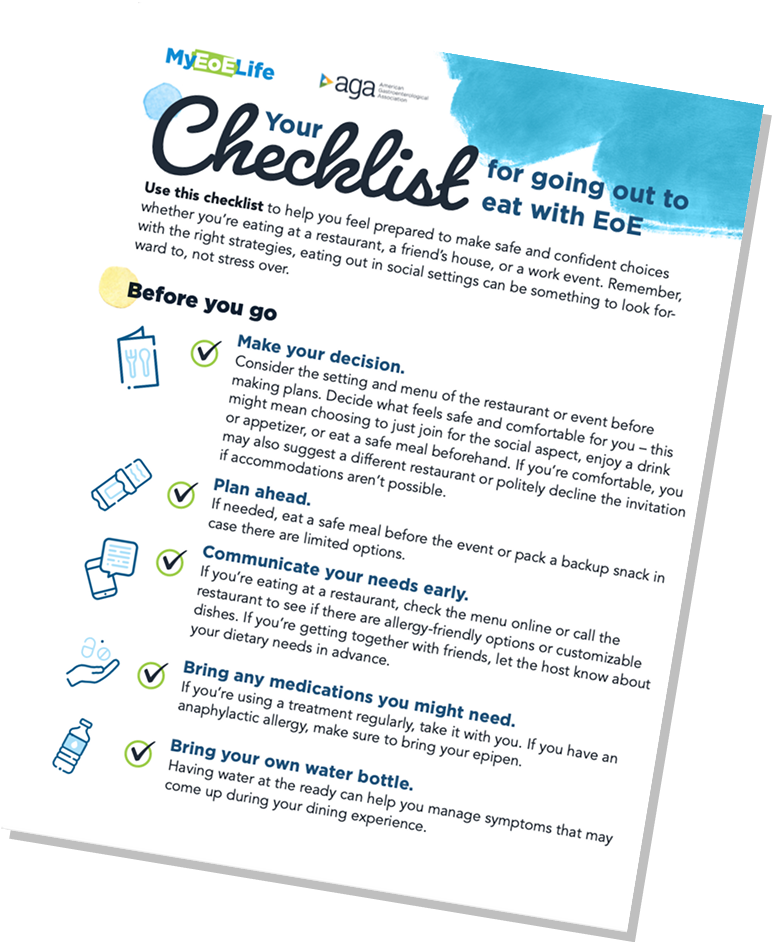
Navigating meals, especially while on dietary therapy for eosinophilic esophagitis (EoE), often means reading between the lines, whether you’re out at a restaurant, grabbing food at a party, or sitting down to a potluck dinner. You might worry about cross-contact, hidden ingredients, or how to explain your needs without feeling like a burden. It can feel overwhelming, but you don’t have to figure it out on your own.
This checklist helps break it down. From what to ask ahead of time to how to talk with hosts, friends, or staff, and what to bring just in case—it’s designed to help you feel more prepared and less stressed. Because sharing a meal should feel like a connection, not calculation.

Everyday life with EoE
Living with eosinophilic esophagitis (EoE) means thinking ahead, like figuring out how to pack medications and safe snacks for a trip, what to say to a roommate about shared spaces, or bringing up your condition on a date without feeling awkward.
This section dives into the moments that don’t always get talked about, with tips and tools to help you plan ahead, set boundaries, and move through daily life with more confidence and less stress.
EoE in school
How students can advocate for themselves and manage EoE in academic life.
Whether you’re figuring out dining hall options, explaining your needs to professors, obtaining and taking medications as prescribed, or navigating social events with food, having the right support for your eosinophilic esophagitis (EoE) can make school feel more manageable and less isolating.
Navigating campus with EoE
Connect with your school’s health or disability services office. You may be eligible for accommodations, including access to a private eating space, allergy-friendly room and kitchen access, flexibility around class absences due to symptoms or procedures, or permission to carry formula or medications during exams.
Talk to dining services. Meet with a staff member to learn more about ingredient labeling, allergen protocols, and whether custom meals or safe prep areas are available. Your school may have a campus dietitian who can support you in this process.
Bring your own food when needed. Whether it’s snacks for long study sessions or meals for group gatherings, planning ahead can make things easier.
Manage your medications. Make sure you have a reliable source to get your medication refills, a place to store them, and the ability to take them regularly with your school schedule.
Creating a supportive environment
Advocate for yourself. If you’re comfortable, let roommates, professors, or classmates know about your condition so they understand how to support you. You don’t need to share everything, just enough to make your needs clear.
Look for student organizations or online communities. Even if there isn’t an EoE-specific group, others managing chronic conditions may share helpful advice, and having a few people who “get it” can go a long way.
Practice the conversations. Whether it’s explaining your dietary or medication needs to a new friend or emailing a professor about a flare, knowing what you want to say ahead of time can help you feel more confident.
EoE at work
Strategies for communication, meal prep, and managing symptoms and medications in professional settings.
There are ways to manage EoE at work without it interfering with your day. A few simple strategies, such as preparing food in advance, taking medications, and having a go-to explanation for coworkers, can make a big difference. The more confident you feel advocating for yourself, the easier it becomes to stay focused and supported on the job.
Accommodations for your needs at work
If EoE affects how you eat, plan, or manage your schedule, it’s worth having a conversation with your employer about what support might help. Reasonable accommodations could include:
- Flexible break times for meals or snacks that align with your eating plan.
- A private or quiet place to take medications or formula if needed.
- Storage space for safe foods or medical nutrition products, such as oral nutrition supplements like Boost or Ensure.
- The ability to opt out of food-centered meetings or events when needed.
- Flexibility around appointments with your gastroenterology provider, allergist, or registered dietitian.
You are protected under the Americans with Disabilities Act (ADA), and EoE may qualify you for accommodations under this law.
How to talk about EoE at work
EoE isn’t widely known, which can make explaining it feel awkward. Our Conversation Starters offer simple language for talking with coworkers, managers, or HR. Practicing what to say can ease pressure and help others understand how to support you.
Managing unexpected office challenges
EoE might not always be visible, but that doesn’t make it less real. From sudden symptoms to food anxiety during office events, here are a few ways to stay prepared:
- Pack an “EoE-friendly” bag that includes safe snacks, medications, or formula you rely on.
- Have a backup plan for days when symptoms flare, whether that’s working from home, taking a break to reset, or rescheduling a meeting.
- Suggest food-free team events when possible or bring something safe that you can enjoy without stress.
- Use shared spaces on your terms. It’s okay to warm up a special meal, use a personal blender, or say no to catered food.
Remember that many people are navigating food sensitivities or health concerns. You’re not alone in setting boundaries. Most coworkers will appreciate your clarity and honesty.
Traveling with EoE
Plan ahead for travel days, flights, or road trips, so you can stay safe and stress-free.
Vacations and getaways should be a chance to relax and enjoy yourself, not stress over what’s on the menu or how your body might react. With a little planning, traveling with eosinophilic esophagitis (EoE) can be both manageable and empowering.
Getting ready for your trip
Talk to your care team before you go. Ask your GI provider and registered dietitian about:
- How to store, travel with, or adjust medications, if needed. Ensure you have enough medication for your travels.
- What safe foods to pack or prepare in advance.
- What to do if symptoms flare while you’re away from home.
Research restaurants and grocery stores near your destination. Look for places that offer allergy-friendly menus or allow for substitutions. Consider calling ahead to ask about accommodations. For more tips, check out our [Going Out to Eat With EoE Checklist].
Pack a travel kit with safe, shelf-stable foods and essentials. Include nonperishable snacks or meals you tolerate well, extra medications, any formula or supplements you rely on, utensils, and basic cleaning supplies if you’ll be preparing food on the go.
Travel with a food plan. If you’re on an elimination diet, make a schedule or checklist to help you stay on track and avoid exposures.
Communicate with your travel group. Let your travel companions know about your dietary needs so they can help you find restaurants or plan meals that work for you.
Carry a doctor’s note. This is especially helpful if you’re traveling with formula, protein-free products, or medications that could raise questions at security checkpoints.
Have a translated description of your condition. If you’re traveling somewhere where you don’t speak the language, bring a short, translated explanation of EoE and your dietary needs.
Locate care nearby. Identify the closest urgent care or hospital, just in case. If traveling internationally, make sure you have travel health insurance that covers chronic conditions.
While you’re away
Know your limits. It’s okay to say no to plans that don’t feel safe. Build in rest time and flexible options so you can enjoy your trip without added pressure.
Stay hydrated, bring a water bottle, and pack layers. While changes in routine and environment can affect EoE symptoms, staying comfortable and nourished is a good way to stay in control.
Insurance coverage and financial assistance
What to know about getting coverage for eosinophilic esophagitis (EoE) care, and where to find financial support resources.
Understanding your insurance options and knowing where to turn for support can help reduce stress, avoid treatment delays, and give you more control over your care.
Understanding insurance coverage for EoE
Coverage can vary widely. Treatments like steroids, biologics, endoscopies, and formulas may require prior authorization or may not be fully covered, depending on your plan and state.
Know your rights. If a treatment or test is denied, you can appeal—and your provider or a patient advocacy group may be able to support you through the process.
Check state mandates. Some states require insurance coverage for elemental formulas, while others don’t. Ask your care team if this applies to you or check with your state’s department of insurance.
Tips for navigating insurance
Ask about coverage before starting treatment. Call your insurance provider to confirm what’s covered, what isn’t, and what steps (like prior authorization) are required.
Work with your providers. Your GI provider or registered dietitian can help explain medical necessity in documentation for appeals or coverage requests.
Keep records. Save all communications with your insurance company, including any denials, appeals, and approvals.
Talk with Human Resources. If you’re insured through your work, your HR team may be able to assist with getting you the right coverage.
Explore cost-saving options. Ask about generics, samples, medication copay or assistance programs, or alternate therapies if costs are high.
Where to find financial assistance
Coverage can vary widely. Treatments like steroids, biologics, endoscopies, and formulas may require prior authorization or may not be fully covered, depending on your plan and state.
Know your rights. If a treatment or test is denied, you can appeal—and your provider or a patient advocacy group may be able to support you through the process.
Check state mandates. Some states require insurance coverage for elemental formulas, while others don’t. Ask your care team if this applies to you or check with your state’s department of insurance.
Copay assistance programs are often available for specialty or biologic medications. Ask your pharmacist or provider for options.
Patient advocacy groups like APFED, EOS Network and CURED Foundation offer insurance guides, financial aid resources, and step-by-step support.
Hospital social workers or financial counselors can help you navigate complex billing, apply for aid, or find nonprofit support.
Planning for transitions in care or coverage
New to adult care? When you turn 18, legal and insurance responsibilities shift. Use AGA’s guide to help you transition from adolescent to adult care. It’s full of tips, information, and advice you can rely on as you get more involved in your own care.
Relationships and intimacy with EoE
How to talk about your condition with partners and navigate the emotional side of chronic illness.
You may be starting a new relationship or navigating intimacy in a long-term one. Either way, living with eosinophilic esophagitis (EoE) can affect how you connect, communicate, and feel about your body.
Even though it’s not always easy to talk about medications, food restrictions, social anxiety, or how symptoms impact your energy or self-image, being open about your needs can strengthen trust, closeness, and support. You learn to speak up, ask for what you need, and build partnerships rooted in empathy, not perfection.
Start with honest communication
Talk about it when you’re ready. There’s no “right time” to share your diagnosis, but when you do, clear, confident communication can help.
Use simple, relatable language. Most people haven’t heard of EoE, so it may help to compare it to food allergies or explain that it’s a condition that causes inflammation in the esophagus triggered by certain foods.
Be specific about your boundaries. Let your partner know if you need to eat at home, bring your own food, skip certain social events, or take breaks to manage symptoms and medications.
Need help starting the conversation? Check out our Conversation Starters for ideas and examples.
Addressing the emotional side
Living with EoE can come with feelings of isolation, anxiety, or frustration, especially when eating is such a big part of social life and intimacy. It’s okay to name these feelings and talk about them with your partner.
You are more than your diagnosis. EoE doesn’t define your worth or your ability to be loved and supported.
Encourage questions. Inviting your partner to learn with you—whether by reading a resource or attending an appointment—can build empathy and strengthen your connection.
Let yourself be seen. Vulnerability can be a bridge to deeper intimacy, not a barrier.
Navigating intimacy on your terms
Not every date has to revolve around food. If shared meals are tricky, create new rituals, like walks, game nights, or music sessions, that help you bond without the stress of eating.
Listen to your body. Fatigue, discomfort, or anxiety can affect intimacy. It’s okay to slow down, adjust plans, or reschedule until you’re feeling more at ease.
Talk about what feels good (and what doesn’t). From energy levels to physical comfort, open dialogue helps your partner support you better.
Seek support if needed. If EoE is affecting your mental health, body image, or relationship satisfaction, a counselor or support group can offer perspective and tools.
Support groups and connecting with others
Find community through online and in-person support networks.
You are not alone. Whether you’re looking for advice, emotional support, or just another person who “gets it,” connecting with others who live with eosinophilic esophagitis (EoE) can be one of the most empowering parts of your journey.
The value of finding your people
Support groups can offer:
Practical tips for managing symptoms, medications, food prep, and navigating healthcare.
A break from isolation. Just knowing you’re not the only one makes a big difference.
A space to ask the questions you might not want to ask your health care providers.
Support for the emotional side of EoE. From anxiety to self-confidence, it helps to hear how others cope and thrive.
How to get involved
Not sure where to start?
- Choose a format: online forum, video support group, or in-person meet-up.
- Join and introduce yourself, or just observe until you’re comfortable.
- Set a goal. Maybe it’s learning more about food trials or connecting with someone your age.
- Respect privacy, ask questions, and share when you’re ready.
Find a support group that works for you
Online communities
You don’t need to leave home to feel connected. These online groups offer a place to ask questions, share wins, and find people who understand life with EoE.
APFED: Forums, Facebook groups, and webinars for all ages.
CURED Foundation: Patient and caregiver forums and learning events.
EOS Network: Advocacy and connection platform for people with eosinophilic disorders.
AGA GI Patient Center: Explore additional AGA-vetted communities and resources.
In-person support groups
Many hospitals and advocacy organizations offer local or regional meetups. Ask your GI provider, registered dietitian, or clinic social worker for recommendations, or explore national directories like those at APFED and EOS Network
Don’t see one near you? Ask your care team how to start your own community.
